Daniel Mirea (October 2025)
NeuroAffective-CBT® | https://neuroaffectivecbt.com
Abstract
In this sixth instalment of the TED (Tired–Exercise–Diet) Series, we explore the neuroscience of sleep and its central role in emotional regulation, cognitive function, and mental health. Sleep is not a passive state but a dynamic neurobiological process that restores metabolic balance, consolidates memory, and recalibrates affective and cognitive circuitry. Drawing on advances in neuroscience, psychoneuroendocrinology, and affective regulation, this article outlines how sleep deprivation disrupts the amygdala–prefrontal network, alters neurotransmitter systems, and amplifies emotional reactivity.
Within the NeuroAffective-CBT® (NA-CBT) framework, sleep represents the “T” in TED, the first pillar of biological stability upon which self-regulation and psychological flexibility depend. Practical guidance for integrating sleep education, circadian rhythm alignment, and behavioural sleep interventions into therapy is provided.
Introducing TED within the NA-CBT Framework
The TED model (Tired–Exercise–Diet) integrates neuroscience, psychophysiology, and behavioural science into a cohesive structure for promoting emotional regulation and biological stability. Within NeuroAffective-CBT®, TED forms the foundation of the Body–Brain–Affect triangle, a conceptual map linking physiology, cognition, and emotion (Mirea, 2023; Mirea, 2025).
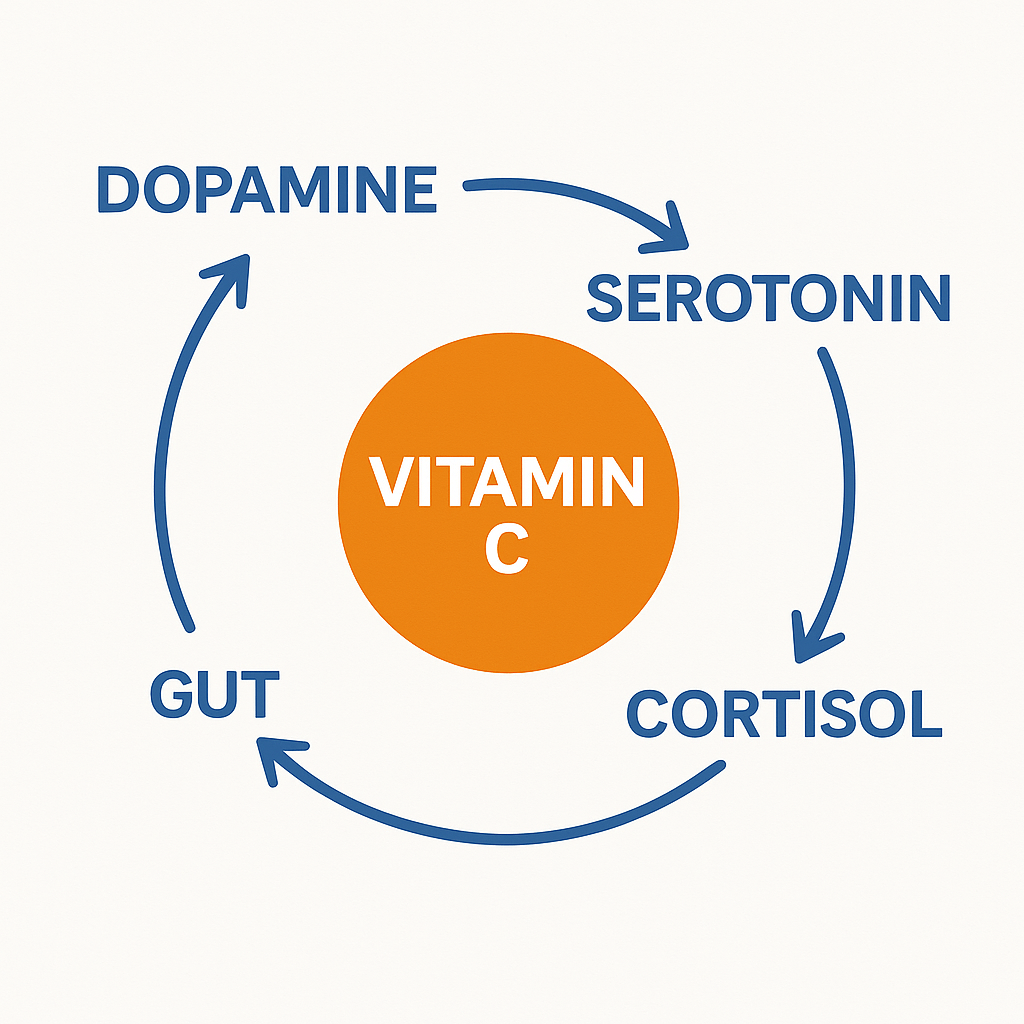
Earlier instalments explored five key nutritional and metabolic regulators of mood and cognition: Creatine (Part I), Insulin Resistance (Part II), Omega-3 Fatty Acids (Part III), Magnesium (Part IV), and Vitamin C (Part V). This chapter returns to the first pillar, Tired, through the lens of sleep neuroscience, affect regulation, and therapeutic practice.
The Science of Sleep and Emotion
Sleep is a biological necessity, not a luxury. Across more than three decades of research, no psychiatric disorder has been identified in which sleep patterns remain normal (Walker, 2017). Disturbed sleep is both a symptom and a cause of emotional dysregulation, stress vulnerability, and cognitive decline.
A landmark neuroimaging study at the University of California, Berkeley, demonstrated that a single night of sleep deprivation increased amygdala reactivity to negative stimuli by 60% (Yoo et al., 2007). Functional connectivity between the amygdala and the medial prefrontal cortex, the brain’s emotional “brake system”, was significantly weakened. Without restorative sleep, emotional responses become amplified and poorly regulated.
Figure 1. The Emotional Brake System
Healthy sleep strengthens communication between the prefrontal cortex (rational control) and the amygdala (emotional response hub). When sleep is lost, this link weakens, leading to impulsivity and emotional hypersensitivity.

The TED Connection
- T – Tired: Adequate sleep keeps the emotional “brake system” intact, balancing reactivity with control.
- E – Exercise: Physical activity enhances sleep quality and increases prefrontal resilience, improving mood regulation.
- D – Diet: Nutrients like magnesium, omega-3s, and vitamin C support neurotransmission and reduce the stress load on emotional circuits.
Together, sleep, movement, and nourishment maintain the brain’s emotional thermostat, preventing small frustrations from turning into major stress responses.
💡TED Translation: Sleep loss disconnects the brain’s emotional accelerator (the amygdala) from its brakes (the prefrontal cortex). When you’re tired, everyday irritations feel bigger and harder to control. Rest, movement, and balanced nutrition keep your emotional “engine” cool and responsive instead of overheated.
The Circadian Code and Homeostasis
Sleep is governed by two intertwined biological systems that keep the brain and body in rhythmic balance:
- The homeostatic drive – the longer you stay awake, the greater the pressure to sleep.
- The circadian rhythm – a 24-hour internal clock, regulated by the suprachiasmatic nucleus (SCN), which aligns your sleep–wake cycles with light and darkness.
When these systems are in sync, the brain functions like a finely tuned orchestra, hormones, temperature, energy, and mood all moving in harmony.
But when artificial light, screens, caffeine, or late-night work override these signals, the rhythm becomes distorted. This mismatch between the body’s internal clock and external demands, known as social jet lag, contributes to fatigue, mood disorders, metabolic changes, and stress dysregulation (Wittmann et al., 2006).
The TED Connection
- T – Tired: Regular sleep and wake times reinforce circadian rhythm and stabilise mood.
- E – Exercise: Morning or daytime movement strengthens the body’s clock by synchronising temperature, cortisol, and energy cycles.
- D – Diet: Eating at consistent times and reducing caffeine or heavy meals in the evening helps align metabolic rhythms with the sleep–wake cycle.
When the TED systems are synchronised, the brain maintains homeostasis, a steady state where energy, hormones, and emotions work together in balance.
💡TED Translation: Your sleep–wake system is like a perfectly timed orchestra. Late nights, bright lights, and random meal times throw the conductor off beat, leading to brain fog, irritability, and poor mood regulation. Keep your rhythm steady with consistent sleep, movement, and mealtimes, and your body will play in tune again.
Sleep and Neurotransmitters
Sleep is among the body’s most powerful regulators of neurochemistry. When we lose sleep, the delicate balance of neurotransmitters that govern mood, motivation, and stress becomes disrupted.
- Serotonin synthesis declines, reducing mood stability and impulse control.
- Dopamine signalling becomes erratic, impairing motivation, pleasure, and focus.
- Cortisol levels rise, keeping the body in a state of chronic alertness.
- GABAergic tone drops, making it harder to relax and fall asleep.
Over time, this imbalance erodes emotional resilience and cognitive clarity. By contrast, adequate and regular sleep restores monoaminergic balance, recalibrates stress hormones, and strengthens the brain’s emotional regulation systems (Goldstein & Walker, 2014).
The TED Connection
- T – Tired: Consistent, restorative sleep keeps neurotransmitters like serotonin, dopamine, and GABA in harmony — your brain’s emotional “chemistry set.”
- E – Exercise: Regular movement boosts dopamine and endorphins, reinforcing motivation and supporting healthy sleep–wake cycles.
- D – Diet: Nutrient-rich foods (omega-3s, magnesium, tryptophan, and B-vitamins) provide the raw materials for neurotransmitter production and recovery.
Together, sleep, movement, and nutrition maintain the neurochemical rhythm that underlies focus, motivation, and mood stability.
💡 TED Translation: When you skip sleep, your brain’s chemistry falls out of tune, more stress, less calm, less focus. Rest, movement, and nourishment reset the brain’s chemical harmony, helping you feel balanced, motivated, and emotionally steady again.
The Immune–Inflammatory Connection
Even partial sleep loss triggers the body’s immune defences as if it were responding to infection. Levels of inflammatory molecules such as interleukin-6 (IL-6) and tumour necrosis factor-alpha (TNF-α) rise, disrupting normal immune balance and leaving the system in a state of chronic, low-grade activation (Irwin & Opp, 2017).
This silent inflammation interferes with neurotransmitters like serotonin and dopamine, fuelling fatigue, irritability, anxiety, and low mood. Over time, a vicious cycle develops: poor sleep increases inflammation, and inflammation in turn further disrupts sleep and emotional regulation.
The TED Connection
- T – Tired: Adequate sleep lowers inflammatory markers, restoring immune and emotional balance.
- E – Exercise: Moderate physical activity reduces systemic inflammation and improves immune resilience.
- D – Diet: Anti-inflammatory foods (omega-3s, magnesium, vitamin C) help counter the stress effects of sleep loss. Alcohol is a highly addictive sedative and a psychological trap, as it convincingly mimics a relaxed state while actually disrupting natural sleep cycles. In contrast, many carbonated (fizzy) drinks act as stimulants, high in glucose and caffeine, which inevitably interfere with restorative sleep.
Together, the TED trio regulates the immune–inflammatory loop, protecting the brain and body from the emotional “wear and tear” of chronic stress and exhaustion.
💡TED Translation: When you don’t sleep enough, your body behaves like it’s under attack. This ongoing silent inflammation drains energy, darkens mood, and keeps your stress system switched on. Rest, movement, and nourishment are your body’s built-in anti-inflammatory medicine.
Sleep, Memory, and Emotional Learning
During REM sleep (Rapid Eye Movement sleep), the brain processes emotional experiences and consolidates learning without reigniting stress responses (van der Helm et al., 2011). This stage of sleep acts as an internal form of overnight therapy, allowing emotional memories to be reactivated, reorganised, and integrated in a calmer physiological state.
Within NeuroAffective-CBT®, this process is vital: therapeutic insights require offline consolidation to transform intellectual understanding into embodied, automatic regulation. In essence, sleep literally “files away” the day’s therapy work, embedding emotional learning into long-term stability.
💡TED Translation: Sleep is therapy’s silent partner. It helps your brain store emotional lessons without reawakening the stress attached to them.
REM sleep is your brain’s emotional reset stage, dream time when the mind replays feelings with the stress dialled down. Think of it as your overnight therapist, quietly helping you process the day, keep the wisdom, and release the worry so you wake up clearer and lighter.
Clinical and TED Practical Guidance
Improving sleep quality is less about effort and more about rhythm, aligning body, brain, and behaviour with the natural cycles that promote restoration. Within the TED framework, each pillar contributes to emotional stability and cognitive resilience through sleep regulation.
T – Tired: Sleep Hygiene and Restorative Rhythm
- Aim for 7–9 hours of sleep each night, ideally aligned with natural darkness (around 10 p.m.–6 a.m.).
- Keep a consistent sleep–wake schedule, even on weekends, to stabilise your internal clock.
- Create a sleep-supportive environment: cool, dark, and quiet spaces enhance deep sleep quality.
- Practice digital hygiene: avoid screens, bright light, and stimulating activities 60–90 minutes before bed to allow melatonin release.
E – Exercise: Movement as a Sleep Stabiliser
- Engage in regular physical activity, ideally during daylight hours, to promote circadian alignment.
- Gentle evening movement such as stretching, yoga or progressive muscle relaxation, can calm the nervous system.
- Avoid vigorous exercise within two hours of bedtime, as it may elevate arousal and delay sleep onset.
- Movement also improves slow-wave sleep, supporting memory consolidation and emotional regulation.
D – Diet: Nutritional Support for Rest and Recovery
- Avoid heavy meals, caffeine, or alcohol within three to four hours of bedtime.
- Prioritise nutrient-rich foods that support neurotransmitter balance: magnesium, tryptophan, omega-3 fatty acids, and vitamin C.
- Maintain consistent meal timing, as irregular eating can disturb circadian rhythm and sleep quality.
- Hydrate well during the day, but reduce fluid intake in the evening to prevent sleep disruption.
Therapeutic Integration
In clinical practice, these habits can be reinforced through cognitive and behavioural interventions for insomnia; techniques such as stimulus control, sleep scheduling, and relaxation training. Within NA-CBT, these methods are integrated with affect regulation, somatic grounding, psychoeducation, and personalised lifestyle adjustments that help clients synchronise biological and emotional rhythms.
💡TED Translation: Good sleep isn’t about trying harder, it’s about working with your body’s natural rhythm. Keep nights dark, meals early, and habits steady. Move during the day, rest at night, and eat in rhythm and your emotional brain will do the rest.
Summary and Outlook
Sleep represents the biological foundation of the TED model; the “T” in Tired, Exercise, Diet. It is the first and most essential pillar supporting affect regulation, learning, and resilience. Within NA-CBT, sleep is viewed as a biopsychological regulator shaping the efficiency of all subsequent therapeutic and behavioural change.
Future TED work should examine how sleep interacts with diet (glycaemic balance, magnesium, vitamin C) and exercise (circadian entrainment, fatigue management), integrating these findings into structured protocols for mood and stress disorders.
Glossary
Amygdala–Prefrontal Network
A key emotional regulation circuit linking the amygdala (the brain’s emotional response centre) and the prefrontal cortex (responsible for rational control and decision-making). Healthy sleep strengthens communication within this network, promoting balanced emotional responses.
Circadian Rhythm
The body’s internal 24-hour biological clock that regulates sleep–wake cycles, hormone release, temperature, and energy levels. It is governed by the suprachiasmatic nucleus (SCN) and synchronised by environmental cues such as light, activity, and mealtimes.
Homeostatic Sleep Drive
The internal biological pressure to sleep that increases the longer one stays awake. Sleep dissipates this pressure, maintaining equilibrium between rest and wakefulness.
NeuroAffective-CBT® (NA-CBT)
A therapeutic framework developed by Daniel Mirea that integrates neuroscience, affect regulation, and cognitive–behavioural methods. It emphasises aligning biological, cognitive, and emotional systems to enhance self-regulation and psychological flexibility.
Progressive Muscle Relaxation (PMR)
A structured relaxation technique that involves tensing and releasing muscle groups throughout the body to reduce physical tension and activate the parasympathetic nervous system. PMR is commonly used to ease anxiety and prepare the body for sleep.
Rapid Eye Movement (REM) Sleep
A distinct phase of the sleep cycle marked by vivid dreaming, rapid eye movements, and heightened brain activity. REM sleep supports emotional processing, memory consolidation, and the integration of affective experiences.
Relaxation Training
A collection of techniques such as, slow breathing, mindfulness, guided imagery, and PMR, designed to reduce physiological arousal and promote calm. Relaxation training activates the body’s “rest-and-digest” system, improving stress recovery and sleep quality.
Sleep Hygiene
A set of behavioural and environmental practices that promote healthy sleep. Core principles include maintaining a consistent sleep–wake schedule, creating a dark and quiet sleep environment, avoiding stimulants before bedtime, and limiting screen exposure in the evening.
Sleep Scheduling
A behavioural intervention for regulating circadian rhythm and improving sleep efficiency. It involves setting fixed bedtimes and wake times, aligning sleep duration with actual sleep need, and gradually adjusting these times to consolidate sleep.
Social Jet Lag
The misalignment between the body’s internal clock and social or work schedules. It commonly arises from late nights, weekend sleep shifts, or irregular meal and activity times, leading to fatigue, mood changes, and metabolic disruption.
Stimulus Control
A behavioural therapy principle aimed at strengthening the association between bed and sleep. It includes going to bed only when sleepy, using the bed solely for sleep and intimacy, rising at the same time daily, and avoiding wakeful activities in bed.
T E D Model (Tired–Exercise–Diet)
An integrative framework within NeuroAffective-CBT® (the third module out of six) linking biological stability with emotional regulation. The model emphasises three foundational pillars, sleep (Tired), movement (Exercise), and nutrition (Diet), as interdependent systems supporting mental health and resilience.
References
Baglioni C et al., 2011. Insomnia as a predictor of depression: A meta-analytic evaluation of longitudinal studies. Journal of Affective Disorders, 135(1–3), pp.10–19.
Goldstein A.N. & Walker M.P., 2014. The role of sleep in emotional brain function. Annual Review of Clinical Psychology, 10, pp.679–708.
Ingram R.E. & Siegle G.J., 2009. Contemporary Issues in Cognitive Therapy. New York: Springer.
Irwin M.R. & Opp M.R., 2017. Sleep health: Reciprocal regulation of sleep and innate immunity. Neuropsychopharmacology, 42(1), pp.129–155.
Mirea D., 2023. Tired, Exercise and Diet Your Way Out of Trouble (TED Model). NeuroAffective-CBT®. Available at: https://neuroaffectivecbt.com [Accessed 27 October 2025].
Mirea D., 2025. TED Series, Part VI: Sleep and Mental Health – The Neuroscience of Restoration and Emotional Regulation. NeuroAffective-CBT®. Available at: https://neuroaffectivecbt.com [Accessed 27 October 2025].
Segal Z.V., Teasdale J.D. & Williams J.M.G., 2018. Mindfulness-Based Cognitive Therapy for Depression. 2nd ed. New York: Guilford Press.
van der Helm E et al., 2011. REM sleep depotentiates amygdala activity to previous emotional experiences. Current Biology, 21(23), pp.2029–2032.
Thayer, J.F. and Lane, R.D., 2000. A model of neurovisceral integration in emotion regulation and dysregulation. Journal of Affective Disorders, 61(3), pp.201–216.
Walker M.P., 2017. Why We Sleep: Unlocking the Power of Sleep and Dreams. London: Penguin Press.
Wells A., 2009. Metacognitive Therapy for Anxiety and Depression. New York: Guilford Press.
Wittmann M et al., 2006. Social jetlag: Misalignment of biological and social time. Chronobiology International, 23(1–2), pp.497–509.
Yoo S.S. et al., 2007. The human emotional brain without sleep – a prefrontal amygdala disconnect. Current Biology, 17(20), pp.R877–R878.
Disclaimer
This article is for educational purposes only and is not a substitute for medical or psychological assessment. Individuals experiencing chronic insomnia or mood disturbances should consult a GP, sleep specialist, or licensed psychotherapist before implementing new interventions.