Abstract
Creatine, long associated with skeletal muscle performance, has attracted growing interest within neuroscience and psychiatry due to its role in cerebral energy metabolism, mitochondrial function, and stress resilience. Evidence from animal models, neuroimaging studies, and early-stage human trials suggests that creatine supplementation may enhance brain bioenergetics, buffer cognitive and emotional functioning under metabolic stress, and augment established treatments for depression when used adjunctively. Preliminary randomised controlled data indicate greater reductions in depressive symptoms when creatine supplementation is combined with cognitive-behavioural therapy compared to psychotherapy alone.
Although findings remain heterogeneous and exploratory, they support a neuroaffective perspective in which cellular energy availability may enable, or constrain, emotional regulation, learning, and psychotherapeutic change. This first instalment of the TED (Tired–Exercise–Diet) series examines creatine as a foundational metabolic substrate within a broader lifestyle neuroscience framework relevant to affect regulation, fatigue, and motivation. The article reviews what creatine is, why it may matter for the emotional brain, and what the current evidence does, and does not, support, while underscoring the need for larger, well-controlled clinical trials prior to routine clinical implementation.
More broadly, this article aims to bridge psychotherapy and lifestyle neuroscience in a grounded, theory-integrative manner, offering relevance to mental health clinicians, researchers, and advanced readers interested in biologically informed approaches to emotional regulation.
Keywords
NeuroAffective-CBT®, TED model, creatine supplementation, lifestyle interventions, affect regulation, shame-based disorders, depression, psychotherapy augmentation, brain energy metabolism, mitochondrial function, fatigue, affect dysregulation
The TED Series: Rationale, Order, and Structure
This article opens the TED (Tired–Exercise–Diet) series, an eight-part examination of how lifestyle-related variables shape emotional regulation, cognitive performance, and mental health. The series addresses not only supplements, but also behavioural and physiological regulators that operate largely outside conscious awareness while exerting significant influence over mood, motivation, self-control, and learning capacity.
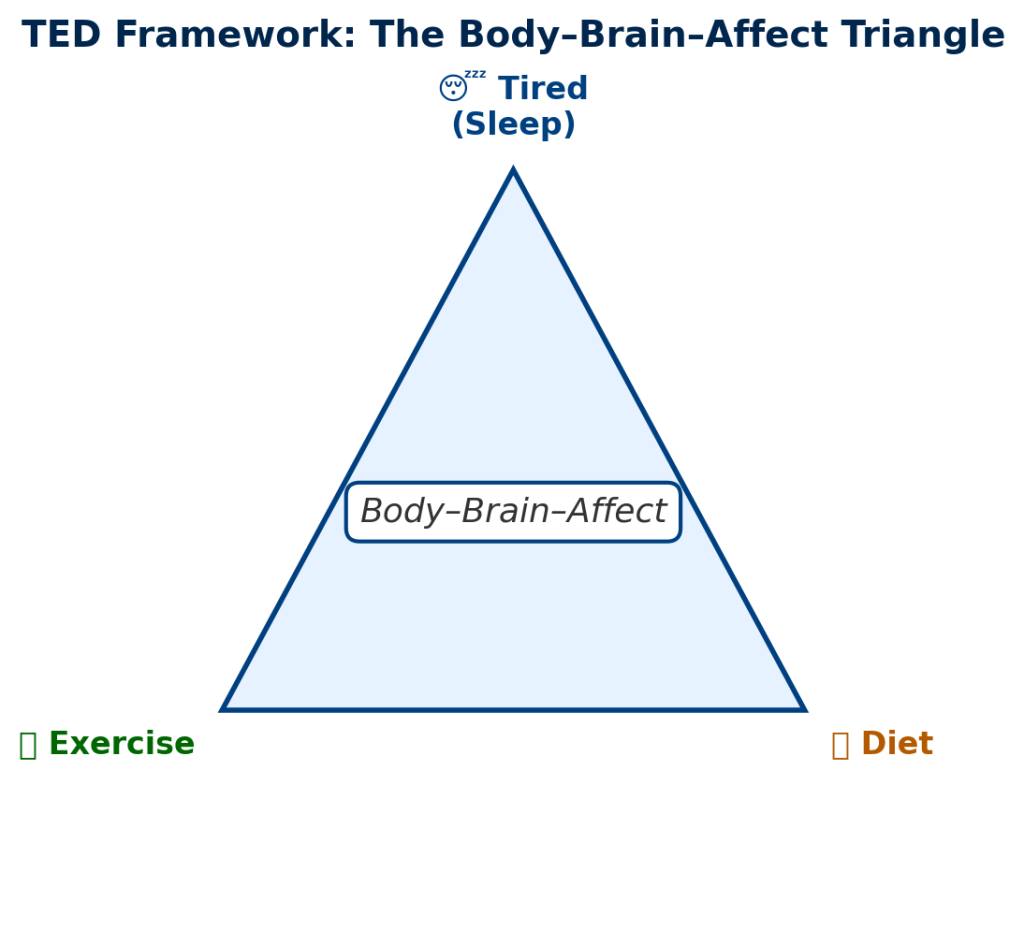
TED is organised around three interdependent pillars:
- T – Tired: sleep, fatigue, circadian rhythm, and recovery
- E – Exercise: movement, strength, metabolic resilience, and stress adaptation
- D – Diet: nutrition, hydration, and gut–brain biochemical signalling
Although conceptually simple, each pillar encompasses multiple interacting neurobiological mechanisms. For this reason, the series both begins and ends with “Diet”. Nutrition supplies the molecular substrates required for neural energy production, neurotransmission, immune balance, and plasticity. Sleep restores and exercise activates; diet sustains the biochemical conditions upon which both depend.
Rather than opening with dietary patterns or prescriptive guidance, Part I focuses on a single, well-characterised nutritional compound central to cellular energy availability. This establishes a physiological foundation upon which subsequent instalments progressively address broader metabolic, neurochemical, behavioural, and restorative processes.
The sequence of the TED series is as follows:
- Part I – Creatine: cellular energy availability and motivation
- Part II – Insulin Resistance: metabolic flexibility and mood regulation
- Part III – Omega-3 Fatty Acids: neuronal membrane integrity and signalling
- Part IV – Magnesium: stress buffering and neural inhibition
- Part V – Vitamin C: antioxidant defence and neurotransmitter synthesis
- Part VI – Sleep: the neurobiology of fatigue and recovery within the Tired pillar
- Part VII – Exercise, Sport Science and Movement: strength, resilience, and stress adaptation
- Part VIII – Diet and “The Hidden Conversation”: how nutrition shapes emotional states
Introducing TED within the NeuroAffective-CBT® Framework
Within NeuroAffective-CBT® (NA-CBT®), TED functions as a biologically grounded scaffold of self-regulation that supports emotional learning, affect tolerance, and therapeutic engagement. Rather than serving as an adjunctive wellness strategy, TED is embedded as a core regulatory module designed to stabilise the physiological conditions upon which affective and cognitive interventions depend.
A central clinical observation underpinning the TED model is that shame-based and affect-dysregulated presentations, characterised by self-loathing, entrenched self-criticism, fatigue, and motivational collapse, frequently co-occur with sleep disruption, metabolic strain, low physical activity, and dysregulated eating. These states are associated with reduced neural flexibility, impaired stress tolerance, and diminished capacity for emotional integration. When such physiological constraints remain unaddressed, engagement with psychotherapy may be limited regardless of insight or motivation.
TED targets three interdependent domains that operate largely outside conscious awareness yet exert powerful influence over mood, motivation, self-control, and learning capacity. Its aim is not optimisation or performance enhancement, but regulation: establishing sufficient physiological stability to widen the window for emotional regulation and psychotherapeutic change.
In NA-CBT®, TED is introduced early in treatment, following assessment and case conceptualisation. Addressing sleep, movement, and nutritional regulation at this stage helps establish the metabolic and neurophysiological conditions necessary for deeper affective and cognitive work. Lifestyle variables are therefore treated as modifiable neuro-behavioural levers capable of influencing dopamine signalling, serotonin synthesis, immune activity, circadian rhythm, and vagus-mediated gut–brain communication.
Daniel Mirea (2023 and 2025) articulated the TED model as “Tired, Exercise, and Diet Your Way Out of Trouble,” positioning it as a bridge between neuroscience, nutritional psychiatry, psychophysiology, and behavioural science. Within this framework, psychological change is constrained, but not determined, by metabolic capacity. TED thus supports, rather than replaces, affect-focused psychotherapy.
In this context, it is important to distinguish the TED framework from performance-first lifestyle or “biohacking” models that prioritise optimisation, productivity, or symptom elimination. Whereas performance-oriented approaches often aim to push cognitive, emotional, or physical output beyond baseline, TED is explicitly regulatory rather than augmentative. Its goal is not to enhance performance, resilience, or motivation per se (although these could be byproducts) but to stabilise the physiological conditions required for emotional tolerance, learning, and self-regulation. Within TED, sleep, movement, and nutrition are not leveraged to maximise efficiency or willpower, but to reduce background physiological noise that constrains affective processing and psychotherapeutic change. In this sense, TED operates as a constraint-reducing framework rather than a performance-enhancing one, supporting psychological work without reframing distress as a failure of optimisation or effort.
What Does the Evidence Suggest.. and What Doesn’t
Creatine has traditionally been viewed as a sports supplement valued for muscular performance. More recently, neuroscience research has examined creatine as a neurometabolic compound relevant under conditions of cerebral stress. Although the liver and brain synthesise small endogenous amounts, supplementation appears most relevant during periods of elevated cognitive demand, sleep deprivation, depression, or neurodegenerative vulnerability, states characterised by energetic strain, inflammation, and oxidative stress.
Animal models, neuroimaging studies, and early-stage human trials suggest that creatine supplementation may enhance brain bioenergetics, buffer cognitive performance under metabolic stress, and support emotional functioning. However, the evidence base remains emergent and heterogeneous, with effects varying by population, dose, and context. Current findings therefore support cautious optimism rather than clinical certainty.
From a NeuroAffective-CBT® perspective, these findings raise the possibility that cellular energy availability may function as a permissive factor for emotional regulation and psychotherapeutic learning, rather than as a direct treatment mechanism.
The Rationale: Bioenergetics, Oxidative Stress, and Brain Demand
Creatine functions as a rapid energy-buffering system, maintaining cellular ATP availability during periods of high demand via the phosphocreatine system. Although commonly associated with muscle tissue, the brain consumes approximately 20% of the body’s resting energy expenditure.
In depression, anxiety, and chronic stress, mitochondrial inefficiency and elevated oxidative stress are frequently observed. These processes are associated with impaired neural signalling, reduced synaptic efficiency, and diminished capacity for affect regulation. By supporting mitochondrial efficiency and stabilising cellular energy availability, creatine supplementation may mitigate some of these constraints.
Animal models demonstrate reduced stress markers and depression-like behaviours following creatine administration, while early human findings remain cautiously promising. Together, these mechanisms suggest a plausible link between bioenergetic support and emotional regulation, although causal pathways remain under investigation.
TED summary: Creatine may help stabilise cerebral energy supply under stress, reducing metabolic interference with emotional regulation and learning.
Human Evidence: Mood, Cognition, and Stress Conditions
Mood and Depression
Controlled trials indicate that creatine may accelerate and potentiate antidepressant effects when used adjunctively. Studies combining creatine with selective serotonin reuptake inhibitors, as well as a recent randomised pilot trial combining creatine with cognitive-behavioural therapy, report greater reductions in depressive symptoms compared to treatment alone, without increased adverse events.
Neuroimaging studies demonstrate increased cerebral phosphocreatine following supplementation, potentially addressing reduced brain-energy states observed in mood disorders. Reviews consistently conclude that creatine shows greatest promise as an adjunct rather than a stand-alone intervention.
TED perspective: By supporting metabolic stability, creatine may enhance engagement with psychotherapy and emotional learning.
Cognition, Memory, and Sleep Deprivation
Systematic reviews suggest that creatine can improve memory, processing speed, and cognitive endurance under conditions of metabolic stress, including sleep deprivation and sustained mental effort. Benefits are most consistently observed in older adults or individuals with compromised energy regulation, while effects in young, well-rested populations are minimal.
Experimental sleep-deprivation models indicate that acute high-dose creatine can reverse cognitive deficits and, in some paradigms, restore performance to near baseline levels. These findings point to relatively rapid effects on cerebral energy metabolism rather than slow structural adaptation.
TED perspective: Creatine may support cognitively and emotionally tired brains under pressure, bridging the Tired and Diet domains.
Key Questions and Practical Considerations
Dose and Brain Uptake
While low-dose creatine (3–5 g/day) effectively supports muscular performance, evidence suggests higher doses may be required to meaningfully elevate brain creatine levels once muscular stores are saturated. Brain uptake appears slower and more variable, which may explain why cognitive and mood effects often emerge gradually. These observations are mechanistic rather than prescriptive.
Electrolytes and Hydration
Creatine transport relies on sodium- and chloride-dependent transporters. Adequate hydration and electrolyte intake may facilitate cellular uptake, although brain-specific effects remain under investigation.
Safety
Extensive evidence supports the safety of creatine monohydrate at standard doses. Rare reports of manic switching underscore the need for monitoring in vulnerable populations, particularly individuals with bipolar spectrum conditions.
Implications for TED and NeuroAffective-CBT®
Creatine should be understood as a supportive metabolic adjunct rather than a substitute for psychotherapy or pharmacotherapy. Its potential value lies in stabilising bioenergetic foundations that may enhance emotional learning, affect regulation, and therapeutic engagement.
From a NeuroAffective-CBT® perspective, insufficient bioenergetic capacity may constrain the brain’s ability to tolerate affect, regulate emotion, and engage in self-reflection. Addressing such constraints may widen the therapeutic window within which affect-focused and cognitive interventions can operate. When integrated within the TED framework—alongside sleep optimisation, structured movement, and nutrient-dense nutrition—creatine may contribute to synergistic effects that support psychological change.
Summary and Outlook
Taken together, current evidence suggests that creatine could play a limited but meaningful role in mental health, not as a stand-alone intervention, but as a metabolic support that may enhance emotional regulation and psychotherapeutic change under conditions of fatigue and stress. Within the TED model, this reflects a broader principle: psychological change is constrained by metabolic capacity. When bioenergetic resources are insufficient, the brain’s ability to tolerate affect, sustain motivation, and engage in emotional learning may be reduced.
By examining creatine in the first instalment of the TED series, this article establishes a physiological foundation for understanding how lifestyle-related variables shape mental health outcomes. Creatine emerges as a scientifically plausible example of how targeted metabolic support may stabilise cerebral energy availability, thereby widening the window within which affect-focused and cognitive interventions can operate. Its value lies in facilitation rather than substitution.
Subsequent instalments examine insulin sensitivity, fatty acid composition, micronutrient sufficiency, sleep architecture, and movement, progressively outlining how lifestyle regulation can support emotional regulation, cognitive flexibility, and neuroplastic change. The final instalment returns to Diet as a whole, reframing nutrition not merely as fuel but as information—a continuous stream of biochemical signals shaping emotional states, cognition, and behaviour. Within this framework, creatine is best understood not as a cure, but as a metabolic ally supporting tired brains so psychotherapy can work more effectively.
⚠️ Disclaimer
These article (like all other NA-CBT articles) is not intended to replace professional medical or psychological assessment or treatment. Lifestyle or supplement changes should always be discussed with qualified health professionals, including a GP, psychiatrist, registered nutritionist, particularly when managing mental health or metabolic conditions.
References:
Allen, P.J., D’Anci, K.E. & Kanarek, R.B., 2024. Creatine supplementation in depression: bioenergetic mechanisms and clinical prospects. Neuroscience & Biobehavioral Reviews, 158, 105308. https://doi.org/10.1016/j.neubiorev.2024.105308
Antonio, J. et al., 2021. Common questions and misconceptions about creatine supplementation: what does the scientific evidence really show? Journal of the International Society of Sports Nutrition, 18(1), 13–27. https://doi.org/10.1186/s12970-021-00412-z
Avgerinos, K.I., Spyrou, N., Bougioukas, K.I. & Kapogiannis, D., 2018. Effects of creatine supplementation on cognitive function of healthy individuals: a systematic review of randomized controlled trials. Experimental Gerontology, 108, 166–173. https://doi.org/10.1016/j.exger.2018.04.014
Braissant, O., 2012. Creatine and guanidinoacetate transport at the blood–brain and blood–cerebrospinal-fluid barriers. Journal of Inherited Metabolic Disease, 35(4), 655–664. https://doi.org/10.1007/s10545-011-9415-6
Candow, D.G., Forbes, S.C., Chiang, E., Farthing, J.P. & Johnson, P., 2022. Creatine supplementation and aging: physiological responses, safety, and potential benefits. Nutrients, 14(6), 1218. https://doi.org/10.3390/nu14061218
Dechent, P., Pouwels, P.J.W., Wilken, B., Hanefeld, F. & Frahm, J., 1999. Increase of total creatine in human brain after oral supplementation of creatine monohydrate. American Journal of Physiology – Regulatory, Integrative and Comparative Physiology, 277(3), R698–R704. https://doi.org/10.1152/ajpregu.1999.277.3.R698
Dolan, E., Gualano, B., Rawson, E.S. & Phillips, S.M., 2018. Creatine supplementation and brain function: a systematic review. Psychopharmacology, 235, 2275–2287. https://doi.org/10.1007/s00213-018-4956-2
Firth, J. et al., 2020. A meta-review of “lifestyle psychiatry”: the role of exercise, smoking, diet and sleep in mental disorders. World Psychiatry, 19(3), 360–380. https://doi.org/10.1002/wps.20773
Harvard Health Publishing, 2024. What is creatine? Harvard Medical School. Available at: https://www.health.harvard.edu/staying-healthy/what-is-creatine
Irwin, M.R., 2015. Why sleep is important for health: a psychoneuroimmunology perspective. Annual Review of Psychology, 66, 143–172. https://doi.org/10.1146/annurev-psych-010213-115205
Kandola, A., Ashdown-Franks, G., Hendrikse, J., Sabiston, C.M. & Stubbs, B., 2019. Physical activity and depression: toward understanding the antidepressant mechanisms of physical activity. Neuroscience & Biobehavioral Reviews, 107, 525–539. https://doi.org/10.1016/j.neubiorev.2019.09.040
Kreider, R.B. et al., 2017. ISSN position stand: safety and efficacy of creatine supplementation in exercise, sport, and medicine. Journal of the International Society of Sports Nutrition, 14, 18. https://doi.org/10.1186/s12970-017-0173-z
L-Kiaux, A., Brachet, P. & Gilloteaux, J., 2024. Creatine for the treatment of depression: preclinical and clinical evidence. Current Neuropharmacology, 22(4), 450–466. https://doi.org/10.2174/1570159X22666230314101523
Lopresti, A.L., 2019. A review of lifestyle factors that contribute to important pathways in depression: diet, sleep and exercise. Journal of Affective Disorders, 256, 38–44. https://doi.org/10.1016/j.jad.2019.05.066
Lyoo, I.K. et al., 2012. A randomized, double-blind clinical trial of creatine monohydrate augmentation for major depressive disorder in women. American
Journal of Psychiatry, 169(9), 937–945. https://doi.org/10.1176/appi.ajp.2012.11081259
McMorris, T. et al., 2006. Creatine supplementation and cognitive performance during sleep deprivation. Psychopharmacology, 185(1), 93–103. https://doi.org/10.1007/s00213-005-0269-8
McMorris, T., Harris, R.C., Howard, A. & Jones, M., 2017. Creatine, sleep deprivation, oxygen deprivation and cognition: a review. Journal of Sports Sciences, 35(1), 1–8. https://doi.org/10.1080/02640414.2016.1156723
Mirea, D., 2023. Tired, Exercise and Diet Your Way Out of Trouble (T.E.D.) model. NeuroAffective-CBT® Publication. Available at: https://www.researchgate.net/publication/382274002_Tired_Exercise_and_Diet_Your_Way_Out_of_Trouble_T_E_D_model_by_Mirea [Accessed 17 October 2025]
Mirea, D., 2025. Why your brain makes you crave certain foods (and how “TED” can help you rewire it…). NeuroAffective-CBT, 17 September. [online] Available at: https://neuroaffectivecbt.com/2025/09/17/why-your-brain-makes-you-crave-certain-foods/ [Accessed 17 October 2025].
Morris, G., Berk, M., Carvalho, A.F. et al., 2017. The role of mitochondria in mood disorders: from pathophysiology to novel therapeutics. Bipolar Disorders, 19(7), 577–596. https://doi.org/10.1111/bdi.12534
Rae, C. & Bröer, S., 2015. Creatine as a booster for human brain function. Neurochemistry International, 89, 249–259. https://doi.org/10.1016/j.neuint.2015.07.009
Silva, R. et al., 2013. Mania induced by creatine supplementation in bipolar disorder: case report. Journal of Clinical Psychopharmacology, 33(5), 719–721. https://doi.org/10.1097/JCP.0b013e3182a60792
Simpson, E.J. & Rawson, E.S., 2021. Creatine supplementation and cognitive performance: a critical appraisal. Nutrients, 13(5), 1505. https://doi.org/10.3390/nu13051505
Sherpa, N.N., De Giorgi, R., Ostinelli, E.G. et al. (2025). Efficacy and safety profile of oral creatine monohydrate as an add-on to cognitive-behavioural therapy in depression: an 8-week pilot, double-blind, randomized, placebo-controlled feasibility and exploratory trial in an under-resourced area. European Neuropsychopharmacology, 90, pp. 28–35.
Tachikawa, M., Fukaya, M., Terasaki, T. & Ohtsuki, S., 2013. Distinct cellular expression of creatine transporter (SLC6A8) in mouse brain. Journal of Cerebral Blood Flow & Metabolism, 33(5), 836–845. https://doi.org/10.1038/jcbfm.2013.6
Zhang, Y., Li, X., Chen, S. & Wang, J., 2023. Creatine and brain health: mechanisms and therapeutic prospects. Frontiers in Neuroscience, 17, 1176542. https://doi.org/10.3389/fnins.2023.1176542