Introducing James…
James is a successful banker enjoying significant authority and respect at work. Being into sports and a healthy lifestyle, he is tall and handsome, he has a beautiful wife and two children. On paper all is well, and so he would be taken by surprise every weekend when visiting his parents’ home for Sunday lunch, by the experience of intense, discomforting, and painful butterflies, in anticipation of this recurring event. He is left confused, without an explanation.
Allowing for an earlier narrative to unfold within the first few hours of therapy, childhood experiences were revealed, where he experienced similar painful feelings, generated by a critical and highly demanding father, the kind of parent that would be difficult to please. His mother never interfered and to James, this was as bad as his father’s attitude. His childhood was dotted with various episodes of unfavourable comparisons with a younger and brighter sister.
Despite his success and handsome appearance, he sees himself as ugly, unattractive, unwanted, enjoying some professional success through sheer luck, an impostor, and a trickster. He remained hypervigilant throughout the years around his father and eager to be validated. He gets overwhelmed with anticipatory anxiety before every single meeting with his parents.
When gently exposed to these issues during therapy, he acknowledged a connection with early experiences right away, he realised that he feels the same way around other men or women in authority, and yet he remained equally confused and troubled by these dominant, painful gut-feelings1.
******
‘I can feel it in my gut‘ or ‘trust your gut’ we often say to ourselves or each other, perhaps for very good reasons. Scientists have recently established clear links between our gut and the brain, not necessarily through an analysis of the diversity of the microbiome that exists within our gut, although this turns out to be equally relevant (Skonieczna-Zydecka K et al., 2018), but also by paying attention to the actual structure of the gut at a cellular level (Kaelberer M et al., 2020).
The biological dimension
Dr Kaelberer and colleagues identified a direct pathway from the gut to the brain, that essentially allows sensing of what is happening in the gut, in order to inform specific emotions whether pleasure or disgust, and the resulting behaviours. This would, at least in part, explain cravings and associated compulsive actions, and furthermore, it helps explain why the regular practising of mindfulness or paying calm, non-judgemental attention inwards, could lead to a shift in feelings and better emotional-regulation (Golding and Gross, 2010).
The gut-brain communication happens through versatile and adaptable neuropod cells with electrical sensors within the gut structure, which are able to select and specialise in various essential chemicals like glucose, proteins or amino acids. These cells can program to organise digestion and send information via electrical signals straight to the brain, which will make further informed decisions on what to feel and how to respond to certain products, in a given situation. Although not the only sensorial command centre, it does appear that, the human 9- to 10-meter-long gut, could be the largest internal organ with immediate access to the external world. Running through the upper body, from the rectum to the esophagus, and in constant communication with the brain, the gut is able to provide an individual, with a fuller experience of what it means to engage with useful edible products, like enjoying a coffee with a cookie in the morning, where the individual is likely to experience both pleasure and a sudden increased in energy. Seems ‘the gut’ may indeed be one of the biggest organs inside our body, but reaching as far as the external or the social world, is not something psychologists would have taken into account until now.
Inside the gut something equally fascinating takes place, which further strengthens the relationship between the human gut and the brain. Our intestine has about 39 trillion microorganisms called microbiome and it consists mostly of bacteria, viruses and fungi – the microbiome produces chemicals which can send messages to the brain through the vagus nerve. This nerve starts in the brainstem, it travels down the neck and alongside the carotid arteries and into the chest branching out towards internal organs, as a result it can manage gut contractions (peristalsis) and heart rate – this makes the vagus nerve relevant when it comes to the human relaxation response.
We now know, that people who suffer from chronic stress have very different microbiomes and ‘bad’ bacteria that produce inflammation, as opposed to a healthy individual who would have a diverse population of bacteria strains. This has serious clinical implications and recent research has in fact shown, that levels of depression would improve when injected with a specific bacteria (faecal). Although these bacteria is proving difficult to reproduce artificially in a lab, the link between the gut micorbiome and the brain explains why certain diets, like the Mediterranean diet, and foods (like pre/probiotics) would have a direct impact on the mood. A healthy diet is associated with a 30% reduction in depression.
Good gut health means good overall health !
The psychosocial dimension
Humans like most other mammals have rituals around eating, drinking and socialising. Such events are usually inter-linked and incredibly important to evolution. Those are ideal occasions to get to know one another, to court each other, to test our emotions, bond and reproduce. Often a potential partner is treated to a freshly cooked meal with a personal touch. This enhances the possibility of having a relationship. Social rituals such as feeding a child, courtship or even kissing, demonstrate how the gut is constantly interacting with the brain and through a perfect symphony of electrical signals, enzymes, and various chemicals, it assists with social bonding, and the selection of the most appropriate partner. This is where the notion of ‘butterflies in the stomach’ takes a completely different meaning when two lovers meet, versus two people shouting at each other in extreme anger. All individuals involved in these very different scenarios, would report experiencing butterflies in the stomach with different levels of intensity. This turns out to be nothing short of cells and electricity at work, dutifully completing their shift. Just another day in the office.
Through stories we reach the world around us…
Homo-sapiens are also ‘homo-narrans’ (Meichenbaum D, 2017). We have an innate ability to observe our own thoughts, to think about our thinking in vivid images, pictures, or even short video clips, and ultimately describe with various details, the content of our thoughts and conclusions. This is what we label as ‘stories’. In fact, we rarely think in clear and brief thoughts, but instead our minds, seem to be dominated by stories involving all sensory modalities, a pleasant memory of a sensual encounter has sounds, smells and tastes, alongside vivid video-reels which unconsciously lead to arousal.
‘The early bird catches the worm’.
We grow up ‘feeding’ on stories, symbols and metaphors; most of us will remember with great pleasure childhood messages and proverbs repeated to exhaustion by our parents and grandparents, in the hope that we would learn to behave more appropriately, in line with our social context and culture. The messages we remember the most, have an interesting narrative behind them, rich in details and sensorial pleasures. The teacher that inspired us during school years, was most likely, the best storyteller. Story telling is a natural gift often unexplored and unnourished.
Stories we tell ourselves reflect earlier experiences and are used as a learning platform. They have to make contextual sense of the world we live in, and as such, our personal narratives, are influenced and adapted over time in order to fit in, with continuously evolving circumstances (Hickes and Mirea, 2012). This would of course, in turn, ensure survivability and psychological resilience over the course of lifetime. Failure to update old narratives can create psychological rigidity, which leads to internal distress and therefore, predispose individuals to mental illness.
Indeed, this fascinating oval-shape mass of grey, which we refer to, as the ‘brain’, is plastic. In other words, it has the ability to biologically modify itself and adapt to new circumstances (another area the conscious mind1 is not consulted about), with only one important mission that supersedes everything else – keeping us alive! Therefore, the stories we tell ourselves are not designed to generate feelings of happiness or sadness, since those are not essential to our survival. Although we know this is at times possible, the brain’s main priority is to keep the organism or the body as a whole, functional and alive.
The cognitive-behavioural dimension
When the gut communicates with the brain, it is purposeful, and it demands an immediate reaction. Intense emotions lead to compulsive behaviours, bypassing the mind completely, e.g., when one is hungry, the resulting senses, known as cravings or feelings of pain and discomfort in the gut area, lead to an urgency to find something to eat, the mind is simply trying to resolve this problem by going to previously memorised solutions.
Therefore, cognitions are products of an extremely busy brain with no time off. Best understood as essential components of a regulatory system informed by thought, experience, memory, language, sensorial data or felt-sense2, and deeply-rooted beliefs3. It may not always be easy, but it is possible to override one’s felt-sense or gut-feelings, if we start engaging our prefrontal abilities by reframing the experience and simply view DRBs as, the dialectical expression of a felt-sense. This can be achieved through new learning, and new experiences. Humans, unlike other mammals, do this all the time, we are very good at convincing ourselves that something is good for us, through repetition or rehearsal, when in fact, our gut is telling us that the opposite is true. For example, eating lots of sugar, drinking alcohol or smoking. In a different context, it could be argued that learning how to override painful gut-feelings, might be the very purpose of a psychotherapeutic treatment specifically, helping individuals overcome painful gut-feelings, or felt-senses which internally suggest they are flawed or not good enough.
Deeply-rooted beliefs might be best understood as the first layer of defence, a deeper screening or filtering system that helps an individual navigate through the complexities of life, in spite of a dominating gut-feeling that he is not good enough. These types of senses are reminders of previous experiences and nothing short of ‘brain statements’ or brain’s best possible interpretation of early life experiences. Whether frequent exposure to extended periods of affection, or at the other end of the spectrum exposure to neglect, characterised by intense pain signals and experienced mostly by the gut, and felt within the upper body regions. Since our brain does not use language per se, to ‘shout out’ warnings to the mind, various electrical signals are sent back and forth between brain structures and different parts of the gut, on every single occasion we find ourselves in a situation that points toward a reward or indeed a threat (i.e., neglect). Sensorial signals alerting an individual of a potential reward or threat, depending on the developmental stage, could be processed linguistically and translated into deeply-rooted beliefs of lovability (pleasure) or unlovability (rejection), but this is rarely needed outside of a therapy session. And of course, lack of awareness and language speeds up the process of getting a reward or running away from neglect or threat. Once the Mind gets involved, everything slows down and is investigated with the curiosity of a scientist.
We have now understood that DRBs are not seen or heard but felt deep inside the body at a gut level and they are not interpreted by a mind which does not even fully develop before the age of two. Therefore, not only that language is not needed when chasing a reward or running away from a threat, but DRBs have no immediate linguistic correspondent, since the gut-brain axis is bypassing the temporal lobe responsible for language processing. Studies suggest that the prefrontal cortex, or the ‘mind’, starts developing within the first two years of life, since basic brain structure and connectivity is present by this age (Huttenlocher & Dabholkar, 1997), but continues until the mid-twenties, which marks an end to our adolescent stage and a slowing down of brain neuroplasticity (Siegel D, 2020).
Attachments and emotional neglect
British developmental psychologist and psychiatrist John Bowlby is one of the most recognisable names associated with attachment research (1988). His evolutionary theory suggests that children come into the world biologically pre-programmed to form attachments with others, since this will help them survive. Indeed, a child that has been emotionally neglected by one of his main caregivers, might not have been a victim of a physically or sexually aggressive parent, nonetheless the child would internalise the absence of warmth and physical affection as threatening, incredibly painful, confusing and difficult to navigate. A child depends for many years on his parents, in order to survive and thrive. And therefore, to a child, the prospect of disappointing a parent is a risky business. Chronically it would be painful, with many types of manifestations and physiological symptoms, like muscle spasms or butterflies inside the body. Not being able to process the experience of rejection or make any sense of it, the gut-brain axis constantly makes decisions on what is healthy and what is not. Eventually these decisions are introduced into our contextual world via stories that we imagine and tell ourselves. These early narratives have implicit deeply-rooted beliefs, not yet linguistically formulated but with clear sensorial messages and themes centred around unlovability, rejection, unworthiness or unacceptability. When finally expressed or spoken ‘out loud’, the language is as varied as individuals’ backgrounds, largely subjected to individuals’ culture, education, imagination and linguistic skills.
Perceived social threats such as criticism and rejection or the prospect of living alone, can be frightening because the gut does not like neglect or going without. Emotional neglect is a real threat in childhood, because it is synonymous with deprivation of essentials, including food and ultimately death. Humans bond to survive. The threat of being alone is basically unbearable to the gut and body by extension.
Deeply-Rooted Beliefs and Contextual-Acceptance
When He says, He is ugly, He also means ‘’The world does not like Me’… and this is the part that really frightens.
It could be speculated that emotional neglect is more impactful on the gut because of the physiological deprivation suffered by the organism. Deprivation of positive affection is associated with lack of appetite or compensatory appetite which leads to the production of specific enzymes and hormones. Whereas, with other types of exerted aggression, the gut suffers less organic deprivation, refocuses on healing, and learns to reprogramme itself allowing for adaption of the whole organism (Kaelberer M, et al., 2020). This could explain why in certain cultures, where physical discipline is widely spread, the actual ‘physical abuse’ does not lead to post-traumatic stress, and it has little or no impact on the immunity and physical health. This type of parenting is not perceived as abusive within the community at large because biologically, it is not significantly harmful, and the emotional dimension is invisible and easier to ignore. The parenting model is therefore normalised, perceived as efficient and often replicated by other families. These sophisticated lines of defence could be viewed as a type of socio-homeostatic process or organism’s attempt to repair and adapt itself through the practice of cultural values and contextual-acceptance.
Deeply-rooted beliefs therefore, may have a regulatory purpose and essentially teach the organism, or the body to adapt.
‘My dad was a little hard on me yesterday, sorry I could not meet you but, I was in a bit of a state’… Friend replies: ‘your dad is fine, you should meet mine… but to be fair, I still hate my homework and love to sneak out for a smoke’.
In a practical sense, to survive and even thrive in, what could be perceived as a harsh environment, requires normalising and acceptance of external living conditions, also coined in this paper, as ‘contextual-acceptance’. Whilst seeing the world through myopic unlovability lenses, James has to adapt to various contexts and whatever else life throws at him, in order to continue to survive and grow in spite of, a dominating felt-sense which strongly suggests he is unappreciated, and likely to be rejected.
‘Since nobody likes me, I have to make more effort than anyone else and behave in ways that will ensure I am safe – despite what everyone really thinks of me’, James would often think to himself, during moments of self-reflection. This type of contextual-acceptance can override the dominating gut-feeling, it leads to psychological adaptation and resilience. When contextual-acceptance is denied, an episode of emotional crisis would be inevitably triggered.
The regulatory quality of deeply-rooted beliefs, also means that they can be accompanied by both negative and positive affective experiences. Someone falling in love or desiring someone sexually feels an acute pain inside the body, within areas of the gut, but this is not registered in a negative manner by the brain and, since it is not a threat, it does not activate fear and avoidance.
By contrast, just thinking about food when hungry can lead to secreting specific enzymes and further compulsive eating behaviours. Going for a driving test can lead to feeling sick in spite of being well prepared. At times, people throw up when faced with social fears and other times they avoid a challenging test all together. It all seems to depend on the lenses the individual uses, because sure enough, when individuals look at the outside world through their unlovability lenses, the whole world would appear likely to reject them, no matter how well behaved they are. It takes effort and motivation to override the gut-feeling. Deeply-rooted beliefs therefore, create myopic lenses but contextual-acceptance heals the pain that comes with it.
Conclusions
Deeply-rooted beliefs have been characterised in the psychotherapeutic literature as schemas by Jeffrey Young (2003) and Paul Salkovskis (1996), core organising principles, often sounding like a code of honour, which the individual cannot afford to break, the cost would be too high, and yet consciously unknown. As such, James’ life was rigidly governed and guided by his unlovability and worthlessness telescope-type lenses.
DRBs are the lenses through which we see the world and ourselves. Supported and confirmed by the gut and with help from specific brain structures, they act as deeply rooted filters, allowing into our consciousness only what the gut-brain-axis feels is relevant to our survival. And as we have already established, the human gut and brain, are not concerned with our happiness or material wealth.
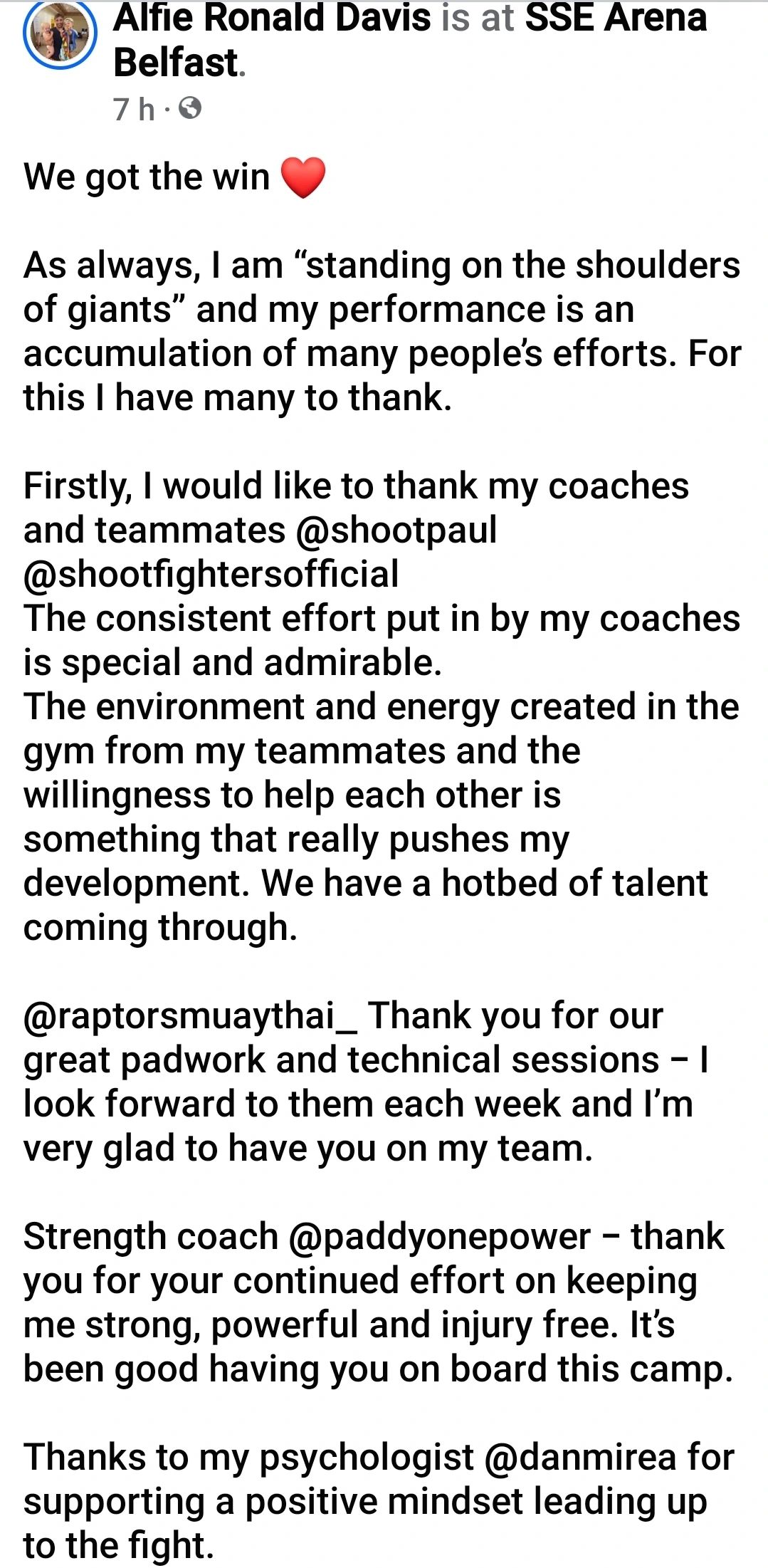
However, the axis is capable of both good and evil and can be persuaded to change and reprogramme the lenses through which we see our life, through an ample process of education and self-awareness, new learning and new coping practices, all key aspects of change. It appears that, just like with any other muscle, all organs inside our body need retraining with consistency over time.
There is nothing more captivating than an authentic story which can send clear motivational messages about meaningful changes and potential solutions. People have been preoccupied with sharing their ideas, personal stories, discoveries, and inventions for thousands of years. Historical writings and drawings on the cave walls are testimony to that fact. Telling ourselves and each other stories, is so embedded within our psychological framework, it has become an essential part of our existence, for where would we be, if it was not for our stories? We tell stories to confirm and justify our very existence.
It appears that stories are very likely, part of our genetical make up and therefore it is not much of stretch to consider that internal storytelling or the narratives we repeat to ourselves, are not only generated, but also perpetuated by our felt-senses or gut-feelings, designed to cement beliefs about who we are, how we could fit into our world, how we need to behave, and what our future prospects are.
Some of our gut decisions are truly worthy of our trust, but we have demonstrated how at times, the gut is misinformed by neglect and emotional deprivation. It falls onto the therapist to guide the patient4 with sensitivity, kindness and compassion, through the sea of vast, often stormy narratives, in order to make sense of the deeply-rooted beliefs’ images, sounds and smells, covert meanings and values.
Perhaps because deeply-rooted beliefs are primarily supporting a survival instinct, those are not always in sync with ideal and current personal values, generated by a fast pacing, ever-changing society. The modern world, the speed of development supported by human creativity, forces us to constantly work on redefining what authentic living means, based on contextual-acceptance.
Whatever this means for each individual, it can only be achieved by constantly refocusing the lenses through which we see ourselves and others, and override deeply-rooted beliefs that support an older way of living or dated values. Charles Darwin, a passionate evolutionary biologist, and author of ‘The origins of species’ (1859) might have been among the first to note that organisms, much like the human organisms with all their guts and brains, would never fail to either adapt or die. It is simply a question of survival.
The ‘Gut – Brain – Affect’ triangle: paving the way to future research and development
Traditionally, psychotherapists have been more interested in the interplay between mind, feelings and actions that lead to ‘psychological pain’ often without being able to answer questions about the subjective feeling of ‘suffering’. Where is all the ‘suffering’coming from, and what are its main characteristics?
The notion of ‘deeply-rooted beliefs’ attempts to answer this dilemma by proposing an investigation into the fascinating world of the ‘gut-brain-affect’ triangle. Searching for answers in an area, that has not been fully explored by psychology just yet, is more than challenging and leads to more questions than answers. At the same time, new and older research studies from physiology, nutrition, attachments, and neuroaffective-biology seem to open a world of therapeutic possibilities.
If the gut and the brain are in constant and autonomous communication (or outside of our awareness), and they make behavioural decisions for us all the time, then it is safe to assume that nutritional and other daily occupational habits, such as the proverbial rest, work, and play, could impact more significantly on our mental health, than ever anticipated (Mirea, 2023). We have always known this instinctively, but the bio-psycho-social processes operating in the background remain a mystery.
This review barely scratches the surface of an intricate world of internal highways of communication, hidden within the human infrastructure, which ultimately leads to behavioural and social decisions, every moment, of every single day. Decisions that ultimately, impact on our wellbeing, quality of life and overall existance.
The article certainly raises more questions than answers, we do not seem to fully understand all the mechanisms that support gut’s constant communication with the brain. But if indeed ‘we are what we eat’ then, psychologists and psychotherapists need to start paying more attention to how nutrition is impacting on our mental health, not just the physical health. Perhaps it falls on the domain of evidence-based psychology to align itself with relevant research from the fields of nutrition, physiology, or neuroscience, in order to better understand the individuals’ relationship with food, digestion, hormones and mental health as well as the environmental impact.
Some progress has been noted in understanding the links between the gut microbiome and depression, but much remains undiscovered and sadly, the psychotherapy community continues to remain silent and uninvolved. This article therefore assumes the risk of going into unchartered territories, potentially exposing many gaps within psychotherapy research. It points toward the sophisticated inner technology of the gut-brain-affect axis with significant implications for mental health treatments. Let’s consider for instance, the relationship between our integumentary system5, emotions, sensations of pain, pain management and mental health. This is an area insufficiently explored within psychology outside of the CBT and Hypno-CBT6 arena.
An example much closer to the subject discussed in this article, would be the potential value of investigating the intestinal chemical formula, that informs us when and if, a product is good for us, and as such, is it worth pursuing in the future. Products consumed are only good, when they are not poisonous for the system, but also when the situation or the context is favourable, in other words, where and when these are consumed. An example would be, when a serious meat eater goes to a new vegetarian restaurant in town that serves an almost too ‘adventurous’ menu for him. On paper this should be a failed event but the ‘context’ takes over completely and so if the individual is in good company, like a date or with someone he actually likes to spend time with, the affective-response changes to joy and pleasure. Through associated learning, a product becomes even more rewarding, and the experience is more likely to be repeated, if the place where the product was discovered, as well as the company kept at the time, were equally rewarding. Culture, existential and personal values, conditioning and social learning theories, memory and language processing, neuroscience, biology and nutrition, all these research domains come into this one simple social experience, which is repeated by tens of thousands of humans every day. Learning theories only partly explain these social decisions and bonding events because, there is an entire domain of the digestive and sensory system that we haven’t even began to articulate in this paper. The same could be said about the links between the digestion system, memory, and language processing. How we describe linguistically an experience, impacts on how we feel about it!
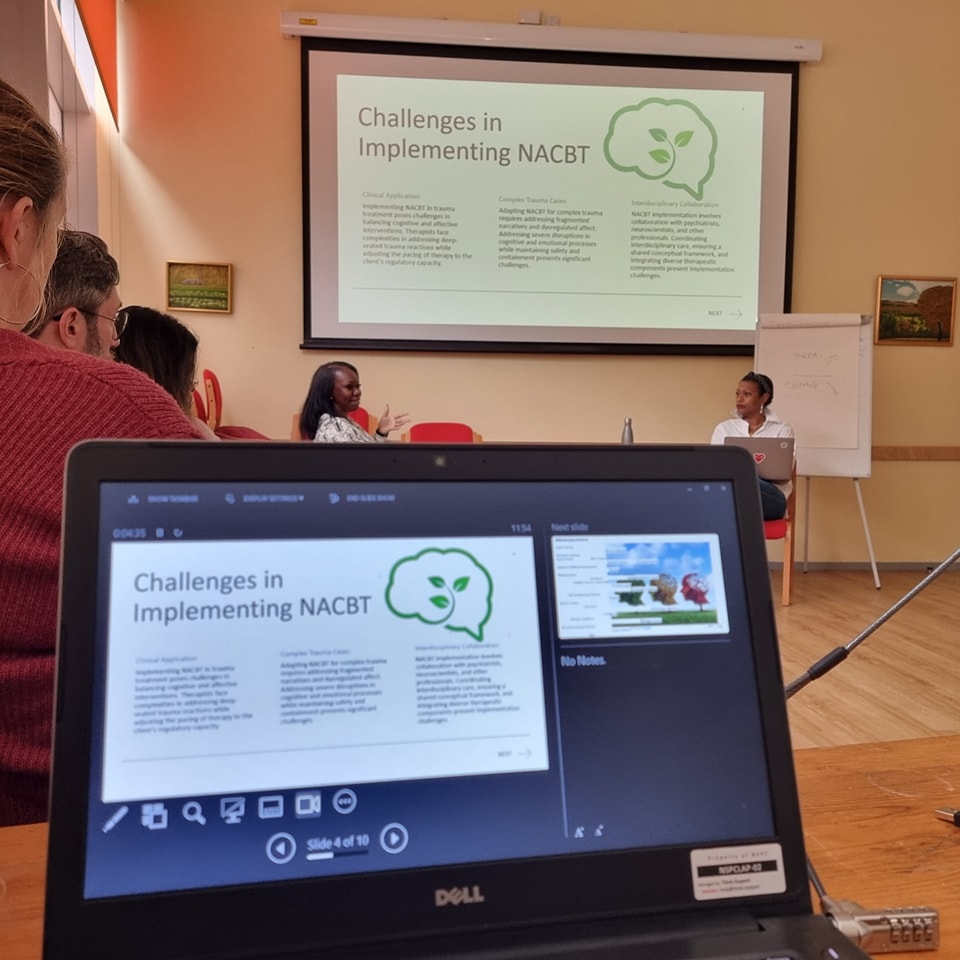
Developing psychotherapy tools such as NeuroAffective-CBT (NA-CBT), which successfully integrates research from all of above mentioned domains, could pave the way for a fourth-wave7 of evidence-based psychotherapy practices (Mirea, 2012). NA-CBT is a transdiagnostic approach, which means that it does not rely on a psychiatric diagnosis and a prescribed treatment protocol, that integrates successfully nutritional advice, physical strengthening programmes, sleep training, and bloodwork analysis (i.e., the TED model, Mirea 2005/2023) alongside traditional behavioural and cognitive interventions. Similarly, future fourth-wave schools of Integrative-CBT8 would aim to improve self-efficacy and enhance individuals’ ability to listen to their bodies, essential skills that claim control over immunity and health overall.
No longer separating the mind from the body in at least, some of the research, might be an obvious step in the right direction. And, perhaps accepting the inevitable – the practice of positive, evidence-based psychology, may be in total contradiction with what we are taught by society that we need, in order to be high achieving and forward moving in life. Modern culture is about learning to override the signals from the body though it seems, at least some of the time, the exact opposite is what humans need. Learning to listen to the signals from the body might be the one of the keys that open the door to healthier living.
Glossary:
1The Mind, or the conscious mind, these terms simplistically refer to higher structures of the brain including the prefrontal cortex (PFC), the section of the brain located behind the forehead; this particular area may be responsible for decision making and finding solutions.
2Felt-Sense, Gut-Sense, Gut-Feelings are senses which act as reminders of previous experiences, designed to alert us of a potential reward or indeed, a threat. These terms are used interchangeably through the paper.
3DRBs: abbreviation for Deeply-Rooted Beliefs. DRBs could be defined as the dialectical expression of (internally experienced) felt-senses, which are translated linguistically later in life when language becomes available, those could in fact, be (verbally) expressed as late as adulthood, often during therapy for the first time. DRBs forge a rigid identity within individuals at an earlier stage in their lives and therefore are harder to modify outside of the therapeutic environment, evidence against DRBs is disregarded through mechanisms like mental filters, described in detail in this paper.
4Patient or Client are the same terms, used interchangeably through the article, usually depends on the situational context or where the therapist is likely to have a practice, at times we refer to our clients as patients or vice-versa.
5Integumentary system refers to the human skin and its structures, the other largest human organ, besides the human gut, which makes up to 16% of the body weight, and also interacts with the external world and further communicates with different parts of the nervous system constantly and autonomously.
6Hypno-CBT – Cognitive Behavioural Hypnotherapy, a transdiagnostic third-wave CBT approach introduced by Donald Robertson and further developed by Mark Davis. Training in Hypno-CBT is offered online and can be accessed here.
7Fourth-wave CBT or the fourth-wave of evidence-based psychotherapy practice refers to the stages of development within the field of evidence-based psychology, CBT in particular. First-wave is marked by extensive behavioural research, this is the foundation of CBT essentially; second-wave brings together research from cognitive psychology and behaviourism; third-wave introduces philosophy and emotional-regulation; fourth-wave is likely to bring along more digital interventions, neuroscience, neurobiology and physiology. For instance, having routinely a blood-test before psychotherapy starts could be considered good practice – since a blood test would point towards physical conditions that have mental health symptoms, like pre-diabetes (Mirea, 2023).
8Integrative-CBT, on short I-CBT was mentioned for the first time at the 9th International Congress of Cognitive Therapy in Transylvania in 2017 @Babes-Bolyai University, event which brought together more than 400 researchers and clinicians from all over the world, event was hosted by Prof. Daniel David, Beck J, Clark D, Hays S and, other renowned clinicians.
REFERENCES:
Bowlby J (1988). A Secure Base: Parent-Child Attachment and Healthy Human Development. Tavistock Professional Book. London Routledge.
Darwin Charles (1859) The origin of Species. Re-edited in 1998 by Jeff Wallace Words world classics literature.
Goldin P and Gross J (2010). Effects of MBSR on emotion regulation in social anxiety disorder. PubMed. Published online Feb 2010. DOI:1037/a0018441. Retrieved on 26/06/2024.
Huttenlocher P.R. and Dabholkar A.S. (1997). Regional differences in Human Cerebral Cortex. Journal of Comparative Neurology, 387, 167-178.
Jacka et al. A randomised controlled trial of dietary improvement for adults with major depression (the ‘SMILES’ trial). BMC Medicine (2017) 15:23.
Kaelberer M.M., Rupprecht L.E., Liu W.W, Weng P, Bohórquez D (2020). Neuropod Cells: Emerging Biology of the Gut-Brain Sensory Transduction. Annual Review Neuroscience. 2020 Jul 8; 43: 337–353. Published online 2020 Feb 26. DOI: 10.1146/annurev-neuro-091619-022657. Retrieved on 26/06/2024.
Meichenbaum D (2017). The evolution of CBT: a personal journey with Don Meichenbaum. Routledge New York and Francis Group.
Meichenbaum D (2010). The roadmap to resilience. Retrieved on 26/06/2024. URL: https://roadmaptoresilience.wordpress.com/
Meichenbaum D (2017). The evolution of CBT: a personal and professional journey with Don Meichenbaum. Routledge, Taylor & Francis Group.
Mirea D and Hickes M (2012). Existential Analysis 23.1. Journal of the Existential Analysis. Jan’12 (p15-31). Retrieved on 28/06/2024. URL: https://www.academia.edu/7069179/CBT_Existential_article_by_Mirea_D
Mirea D (2012). Cognitive Behavioural Coaching, friend or foe – in Existential Perspectives on Coaching edited by Emmy Van-Deurzen and Monica Hanaway. Pallgrave Macmillan. Retrieved on 28/06/2024. URL: https://www.academia.edu/10757925/Existential_Perspectives_on_Coaching_CBC_friend_or_foe_to_the_existential_coach
Mirea D (2018). CBT, whats all the fuss about? Retrieved 29/06/2024. URL: CBT, what’s all the fuss about ? – NeuroAffective-CBT (neuroaffectivecbt.com)
Mirea D (2023). Tired, Exercise and Diet your way out of trouble, TED is your best friend. Retrieved 29/06/2024. URL: Tired, Exercise and Diet your way out of trouble, TED is your best friend ! – NeuroAffective-CBT (neuroaffectivecbt.com)
Rachelle S. Opie, Adrienne O’Neil, Felice N. Jacka, Josephine Pizzinga & Catherine Itsiopoulos (2018)A modified Mediterranean dietary intervention for adults with major depression: Dietary protocol and feasibility data from the SMILES trial, Nutritional Neuroscience, 21:7, 487-501.
Robertson D (2013). The practice of Cognitive-Behavioural Hypnotherapy. Routledge. Taylor & Francis Group.
Salkovskis P (1996). Frontiers of Cognitive Therapy. The Guildford Press New York London.
Serafini G. Neuroplasticity and major depression, the role of modern antidepressant drugs. World J Psychiatry. 2012;2(3):49-57. Duman CH, Duman RS. Spine synapse remodeling in the pathophysiology and treatment of depression. Neurosci Lett. 2015;601:20-9.
Siegel D (2020). The developing mind (3rd edition). The Guildford Press New York London.
Skonieczna-Żydecka K, Marlicz W, Misera A, Koulaouzidis A (2018). Microbiome—The Missing Link in the Gut-Brain Axis: Focus on Its Role in Gastrointestinal and Mental Health. Journal of Clinical Medicine. Retrieved 26/06/2024. URL: https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7573801/
Yang CC, Barrós-Loscertales A, Pinazo D, et al. State and training effects of mindfulness meditation on brain networks reflect neuronal mechanisms of its antidepressant effect. Neural Plast. 2016;2016:9504642.
Young J, Klosko J, Weishaar M (2003). Schema Therapy. The Guildford Press New York.
Roma Pahwa; Amandeep Goyal; Ishwarlal Jialal (2023). Chronic Inflamations. National Library for Medicine, URL: https://www.ncbi.nlm.nih.gov/books/NBK493173/#:~:text=Introduction,%5D%5B2%5D%5B3%5D
Main papers and online research retrieved during June 2024:
Articles – NeuroAffective-CBT (neuroaffectivecbt.com)
M. Maya Kaelberer, PhD | Center for Gastrointestinal Biology and Disease (unc.edu)
Acknowledgements:
This article could not have been finished without valuable guidance and input from Dr Donald Meichenbaum. Dr Meichenbaum is considered by most the ‘Freud of CBT’, one of the three main pioneers, alongside Aaron T Beck and Albert Ellis, of early cognitive and behavioural therapies. Dr Meichenbaum subsequently played an instrumental role in understanding violent trauma, aggressive behaviours, and human resilience.
Editing by Dr D Meichenbaum, SIT and CBT founder; proof reading by Ana Ghetu psychosocial researcher and Dr S Reilly clinical researcher and general practitioner.