Daniel Mirea (October 2025)
NeuroAffective-CBT® | https://neuroaffectivecbt.com
Abstract
In this fifth instalment of TED (Tired–Exercise–Diet) series, of the NeuroAffective-CBT® project, we explore the multifaceted role of Vitamin C in mental health. Emerging evidence suggests optimal neurocognitive benefits occur at daily intakes of 200–500 mg. Beyond its reputation as an immune booster, Vitamin C functions as a key modulator of neurotransmitter synthesis, oxidative stress, and immune–brain communication. Drawing on recent research in neuroscience, nutritional psychiatry, and psychoneuroimmunology, this article examines how Vitamin C supports emotional regulation, cognitive performance, and resilience under chronic stress. Integrating this evidence within the NeuroAffective-CBT® (NA-CBT) framework, we highlight Vitamin C as a practical component of lifestyle-oriented psychotherapy, bridging nutrition, physiology, and affect regulation.
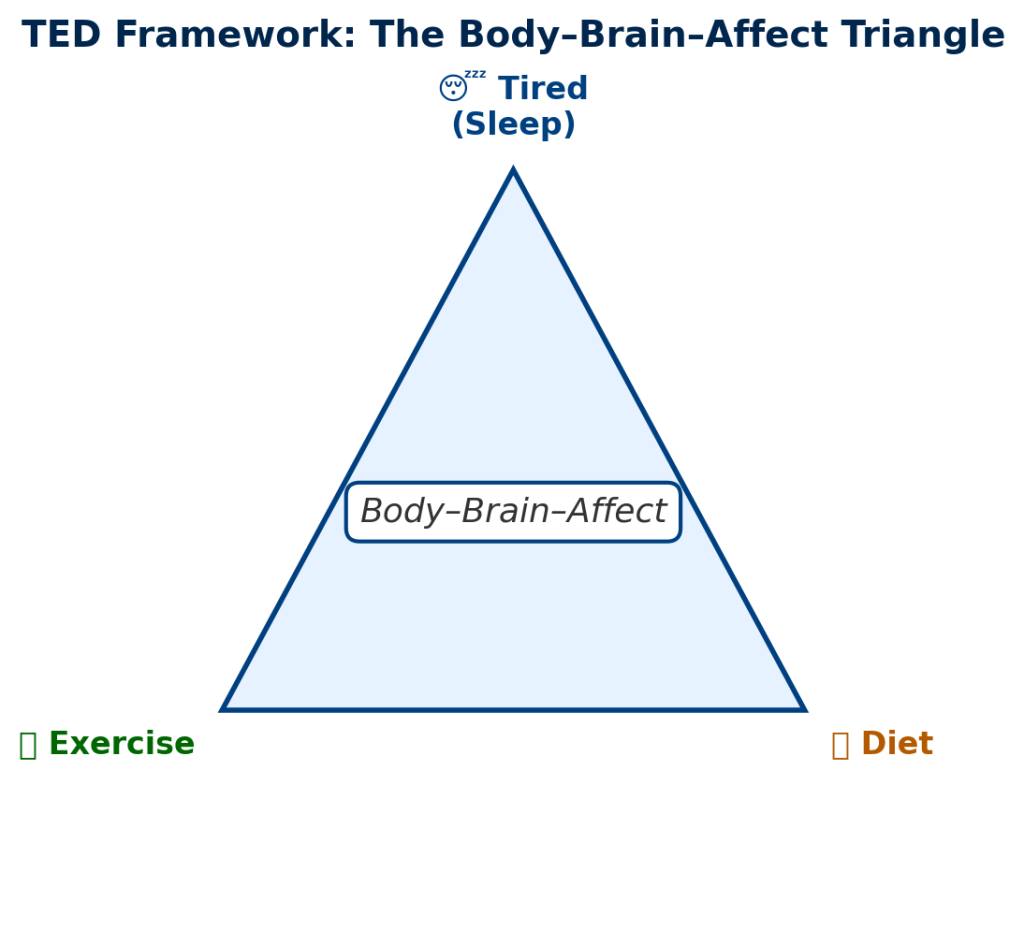
Introducing TED in the NeuroAffective-CBT® Framework
The TED model (Tired–Exercise–Diet) synthesises neuroscience, psychophysiology, and behavioural science into an integrated scaffold for emotional regulation and biological stability. Within NeuroAffective-CBT®, TED interventions are introduced early in therapy to restore homeostasis across the Body–Brain–Affect triangle, the physiological foundation of affective regulation, motivation, and self-concept (Mirea, 2023; Mirea, 2025).
Following earlier TED instalments on Creatine (Part I), Insulin Resistance (Part II), Omega-3 (Part III), and Magnesium (Part IV), this chapter focuses on Vitamin C, a micronutrient that bridges diet, stress, immunity, and cognition. Despite being essential to brain and body function, humans have lost the genetic capacity to synthesise Vitamin C, making dietary intake or supplementation critical for maintaining mental and metabolic health.
Evolutionary Context: A Necessary Deficiency
Unlike most mammals, humans lack the gulonolactone oxidase gene required for endogenous Vitamin C synthesis. Evolutionarily, this was likely pruned due to ancestral diets rich in fruits and vegetation (Harrison & May, 2009). Consequently, Vitamin C must be obtained through food, primarily fruits, vegetables, and, more recently, supplementation.
This evolutionary dependency aligns with human dietary anatomy: our dentition and digestive tract are optimised for plant-based, nutrient-dense foods rather than raw animal flesh. Thus, our reliance on Vitamin C-rich diets is biologically hardwired, linking nutrition directly to both immune and psychological resilience.
From a TED perspective, this represents a fundamental Diet–Affect relationship: emotional and physiological stability rely on the consistent intake of nutrients we cannot make ourselves.
Vitamin C and Neurotransmitter Synthesis
Vitamin C plays a pivotal biochemical role in neurotransmitter regulation. It acts as a cofactor for dopamine β-hydroxylase, the enzyme converting dopamine into norepinephrine (adrenaline), essential for motivation, attention, and stress response (Otte et al., 2016). It is also necessary for the metabolism of tryptophan into serotonin, the neurotransmitter most associated with emotional regulation and well-being (Young, 2020).
Low Vitamin C levels have been linked to reduced serotonin and norepinephrine activity, contributing to low mood, fatigue, and anxiety. In turn, adequate Vitamin C enhances the synthesis and stability of these neurotransmitters, improving energy and affective balance.
💡 TED Translation:
Vitamin C acts as a “biochemical connector” in the Tired and Diet domains, fuelling the brain’s ability to convert nutrients into emotion-regulating signals. When Vitamin C is low, dopamine and serotonin pathways slow down, leading to fatigue, irritability, and low resilience under stress.
Stress, Cortisol, and Oxidative Load
Vitamin C is among the most concentrated antioxidants in the brain and adrenal glands, the latter being the body’s cortisol-producing centres. Chronic psychological or physical stress depletes Vitamin C rapidly, while low Vitamin C status impairs the body’s ability to modulate cortisol output (Brody et al., 2002).
Experimental studies show that supplementation can reduce stress-induced cortisol elevations and improve mood under high-pressure conditions, such as academic or occupational stress (de Oliveira et al., 2015). The relationship is reciprocal: stress depletes Vitamin C, and deficiency heightens the physiological stress response.
💡 TED Translation:
This is where Tired meets Diet: stress “burns through” Vitamin C reserves, and depletion feeds back into higher cortisol and anxiety. Maintaining adequate Vitamin C helps keep the stress response efficient rather than overreactive.
Vitamin C, Immunity, and the Gut–Brain Axis
Vitamin C supports both innate and adaptive immunity, promoting leukocyte function, barrier integrity, and antioxidant defence (Carr & Maggini, 2017). Its influence extends to the gut–brain axis, the bidirectional communication between intestinal microbiota and the central nervous system.
Figure 1: The Vitamin C–Neurotransmitter–Stress Interaction Loop
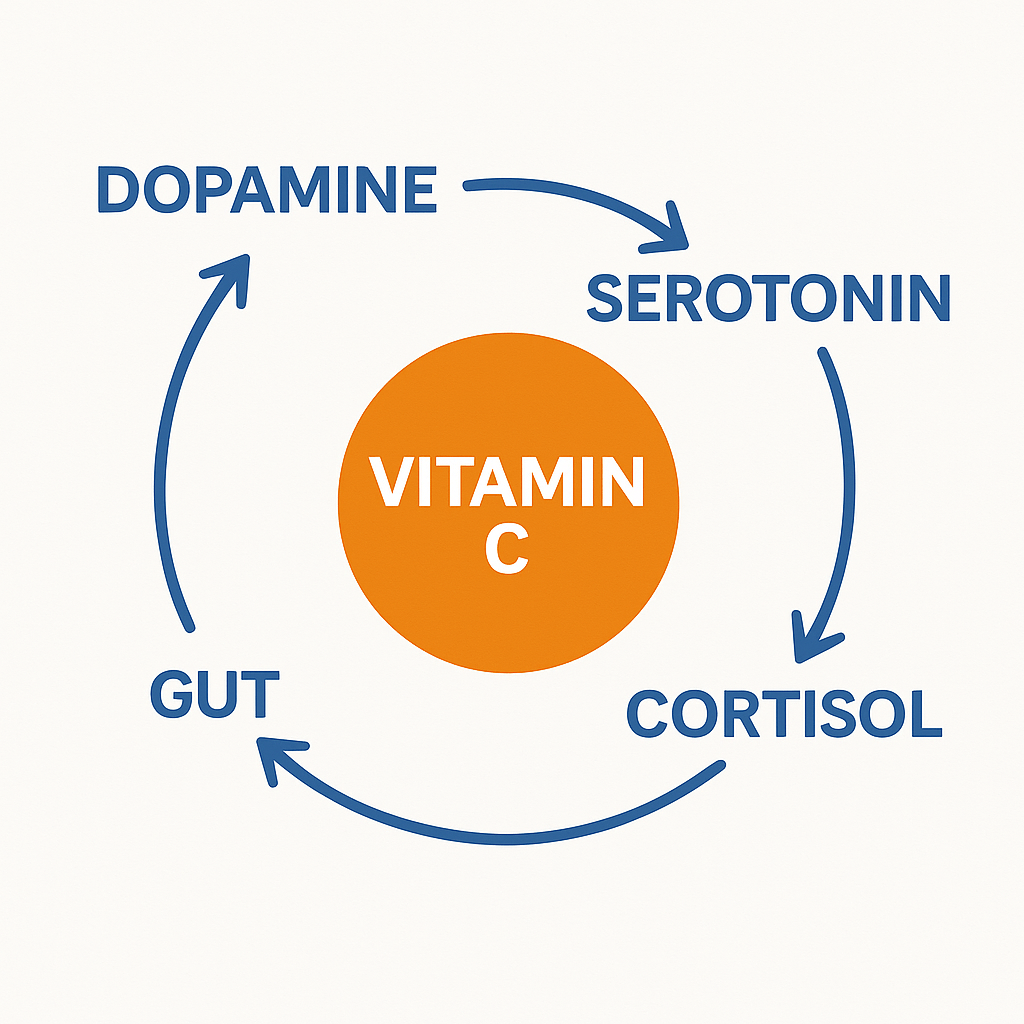
Deficiency in Vitamin C increases intestinal permeability (“leaky gut”) and systemic inflammation, which can trigger neuroinflammatory cascades linked to depression and anxiety (Otte et al., 2016). Adequate Vitamin C intake may therefore modulate mood indirectly by maintaining gut integrity and reducing inflammatory load.
💡 TED Translation:
Within TED, Vitamin C stabilises both the body and the mind, supporting the “Diet” domain by maintaining gut health and the “Affect” domain by reducing the inflammatory signals that disrupt mood regulation.
Epigenetic and Cognitive Dimensions
Emerging research suggests Vitamin C contributes to epigenetic regulation, influencing DNA methylation and histone modification processes involved in early neurodevelopment and long-term emotional outcomes (de Beni et al., 2021).
High concentrations of Vitamin C are found in the brain and cerebrospinal fluid, particularly in the hippocampus and cortex, regions essential for memory and emotional learning. Even when blood levels fall, the brain retains Vitamin C preferentially, highlighting its role in preserving neurocognitive function under stress.
💡TED takeaway:
Your brain treats Vitamin C like gold, it holds onto it even when the rest of your body runs low. That’s because Vitamin C helps protect brain cells, supports memory, and keeps emotional circuits flexible under stress. New research shows that Vitamin C doesn’t just work in the moment, it may even influence how certain genes involved in brain development and emotional balance get “switched on” or “off.” In simple terms, Vitamin C helps your brain stay adaptable, protecting your mood and mental sharpness over time. In TED language, vitamin C fuels both Diet and Affect, nourishing your brain’s chemistry while helping it handle life’s stress without burning out.
Clinical and TED Practical Guidance
Recommended dietary intake for adults is 75–90 mg/day, but emerging data suggest higher doses (200–500 mg/day) may optimise antioxidant and neurochemical benefits (Carr & Rowe, 2020).
Natural sources:
- Citrus fruits (orange, lemon, grapefruit)
- Kiwi, strawberries, papaya
- Bell peppers, broccoli, spinach, kale
Supplementation:
- Divide doses (e.g., 250 mg twice daily) for better absorption.
- Combine with flavonoid-rich foods (e.g., berries, green tea) to enhance bioavailability.
- Avoid smoking and chronic alcohol use, which accelerate Vitamin C depletion.
💡TED Translation:
Think of Vitamin C as your brain’s “daily maintenance nutrient”, keeping neurotransmitters balanced, inflammation low, and energy steady. Consistent intake, alongside sleep and exercise regulation, reinforces the biological base for emotional stability and therapeutic progress. This is such a vital hormone, clinicians may consider psychoeducating clients on Vitamin C’s stress-buffering role when addressing fatigue or anxiety, integrating nutritional discussions within TED-based behavioural activation plans.
Summary & Outlook
Vitamin C exemplifies the TED principle that emotional health begins with biological balance. It supports neurotransmitter synthesis, moderates stress responses, protects against oxidative damage, and sustains gut and immune integrity. Within NeuroAffective-CBT®, Vitamin C functions as both a preventive and adjunctive intervention, enhancing emotional resilience and amplifying the effects of psychotherapeutic change.
Like Omega-3, Magnesium, and Creatine in earlier TED modules, Vitamin C represents a key neuro-metabolic pathway where diet and mood converge. However, supplementation should never replace clinical care, it must be introduced under professional guidance and viewed as a supportive component of comprehensive mental health treatment.
Emerging evidence suggests that optimal neurocognitive benefits occur at daily intakes of 200–500 mg of slow release (or time release) Vitamin C, the type that stays longer in the system. Future research should explore Vitamin C supplementation within structured TED protocols for mood, stress, and cognitive disorders, bridging nutritional neuroscience with applied behavioural interventions.
⚠️ Disclaimer
These articles are for educational purposes only and do not replace medical or psychological evaluation. Individuals should consult their GP or prescribing clinician before starting supplementation, especially if taking psychiatric or cardiovascular medication.
Series context: Mirea, D. (2025) TED Series, Part IV: Magnesium and Mental Health. NeuroAffective-CBT®. Available at: https://neuroaffectivecbt.com/2025/10/21/ted-series-part-iv-magnesium-and-mental-health/ [Accessed 22 October 2025].
References
Brody, S., Preut, R., Schommer, K. and Schürmeyer, T. (2002) ‘Vitamin C high-dose supplementation reduces anxiety and cortisol levels’, Psychopharmacology, 159(3), pp. 319–324.
Carr, A.C. and Maggini, S. (2017) ‘Vitamin C and immune function’, Nutrients, 9(11), 1211.
Carr, A.C. and Rowe, S. (2020) ‘The emerging role of vitamin C in health and disease’, Nutrients, 12(9), 2736.
de Beni, R. et al. (2021) ‘Vitamin C and epigenetic regulation of brain development and function’, Frontiers in Neuroscience, 15, 690341.
de Oliveira, I.J. et al. (2015) ‘Effects of oral vitamin C supplementation on anxiety in students: A double-blind, randomized, placebo-controlled trial’, Pak J Biol Sci, 18(1), pp. 11–18.
Harrison, F.E. and May, J.M. (2009) ‘Vitamin C function in the brain: vital role of the ascorbate transporter SVCT2’, Free Radical Biology and Medicine, 46(6), pp. 719–730.
Mirea, D. (2023) Tired, Exercise and Diet Your Way Out of Trouble (TED Model). NeuroAffective-CBT®. ResearchGate.
Mirea, D. (2025) TED Series, Part IV: Magnesium and Mental Health. NeuroAffective-CBT®. Available at: https://neuroaffectivecbt.com/2025/10/21/ted-series-part-iv-magnesium-and-mental-health/ [Accessed 22 October 2025].
Otte, C., Gold, S.M., Penninx, B.W. et al. (2016) ‘Major depressive disorder’, Nature Reviews Disease Primers, 2, 16065.
Young, S.N. (2020) ‘Tryptophan metabolism and serotonin synthesis: relevance for psychiatric disorders’, Journal of Psychiatry & Neuroscience, 45(3), pp. 151–161.