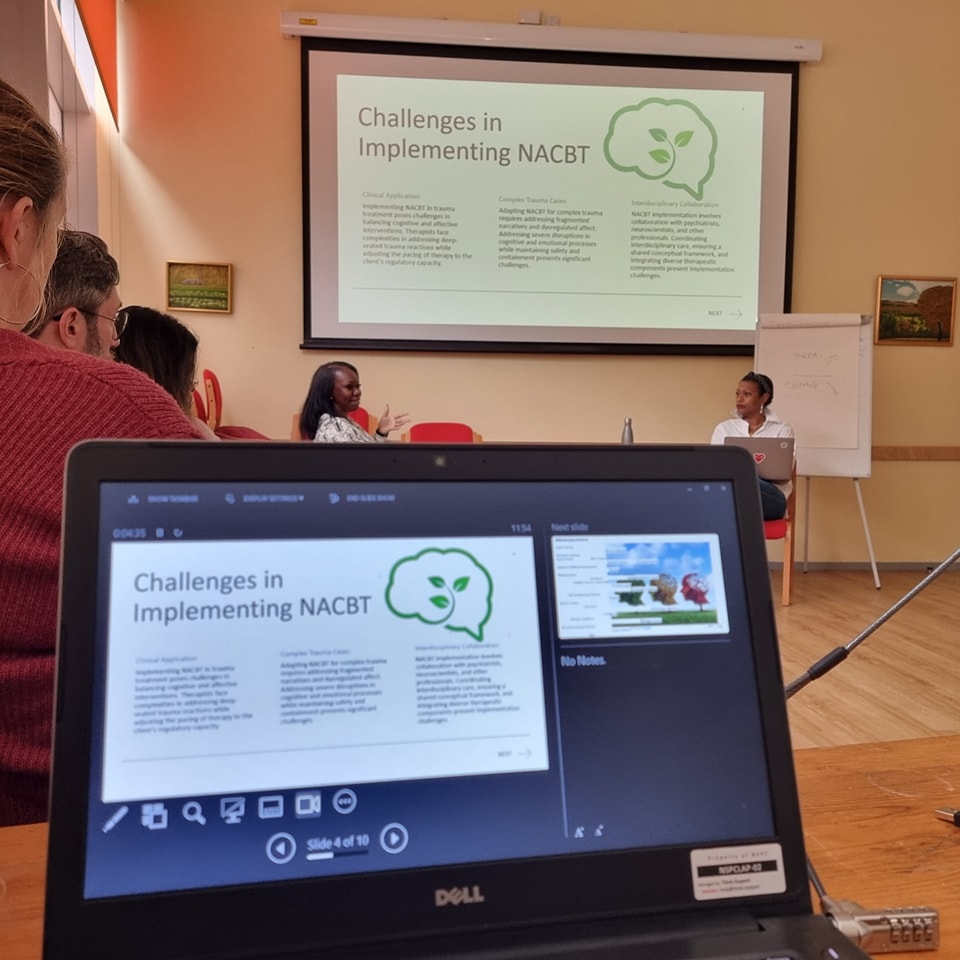
Well.. most rumours are actually true. At least according to Frontiers of Psychiatry (the January 2018 edition) CBT is the gold standard in the field of psychotherapy, because of its clear research support and continuous development and improvement based on research findings. It presently dominates the international guidelines for psychosocial treatments, making it a first-line treatment for most disorders, as noted by the National Institute for Health and Care Excellence’s guidelines 2 and American Psychological Association.3
This is no longer the new kid on the block, even though it was the latest to join in at the big boys table in the mid-60’s. Back then, CBT was merely a treatment protocol for depression written by the brilliant Aaron Tim Beck an analytically trained psychiatrist. The clinical world soon realised that this new kid nicknamed by Beck CBT, is here to stay and might even attempt to take over. So much so that today, we are talking about CBT being an umbrella term for a number of therapies or approaches with many strange names but a clear task to treat a variety of different psychiatric disorders (i.e. Schema Therapy, SIT, PE, MCT, MBCT, DBT, ACT, CFT and a lot of other acronyms).
CBT is a pretty fast paced, short-term, modern therapy with flexible therapeutic boundaries. Yes that’s correct fellow therapists, behaviourists have always steered away from traditional psychotherapeutic boundaries – in my humble opinion, these dated boundaries are probably still rooted in an unworkable Freudian-psychoanalytical approach. I am sure this is a gross exaggeration, but nonetheless it does not change the fact that CBT does not necessarily adhere to the traditional therapeutic boundaries. Whilst some therapists still wonder over the usefulness of shaking hands with their patients or comforting someone crying, we stick our hands down the toilet to demonstrate to our OCD patients that germs don’t instantly kill.. and then we shake their hands! Sessions can take place in the comfort of a clinic (if we are lucky enough) or in patient’s residence or outdoors or at patient’s work place. It all depends on the type pf exposure exercises or social experiments that we would have agreed on, in advance, with the patient.
The formal term used in CBT is ‘collaboration’. Indeed CBT therapists collaboratively agree on most, if not all, social experiments and treatment goals, but the clinical reality and the level of chronicity faced in therapy, often demand an approach that is more direct, symptoms focus, problem-solving and goal oriented, relying on a lot of teaching and a clearly prescribed, evidence-informed treatment plan facilitated by an expert therapist (‘expert’ in mental health problems and potential solutions, not in clients’ lives). The therapy methods used, from exposure to cognitive restructuring, are steeply rooted in behaviourism, learning theories and even physiology. The works of Skinner BF, Watson J, Pavlov I, Jacobson E, Salters A and a few other creative but not always popular (or even ethical by today’s standards) behavioural psychologists from the beginning and middle of the 20th century, form a solid foundation for all CBT approaches.
Nowadays cognitive-behavioural practitioners describe methods which evolved over years of research in three distinct waves of CBT. There are whispers about a fourth wave even. The first wave is steeped into the experimental work and research of early behaviourists, the second-wave was kicked off by pioneers such as Aaron T Beck, Albert Ellis and Donald Meichenbaum, this is when the term ‘CBT’ begins to stand out in both research and clinical practice, in fact this would be ‘the CBT’ that most people are familiar with and challenge in research to this day.
Third-wave CBT is marked by a slight departure from earlier methods with the arrival of imagery-based and philosophically informed approaches such as mindfulness and acceptance therapy. The family of CBT therapies is rather large today and packed with acronyms such as MBCT, DBT, ACT, CFT, etc. Even though though mindfulness, acceptance and compassion-based therapies are associated with the Buddhist philosophy it is important to acknowledge that the main drivers that underpin these methods, developed by true visionaries like Jon-Kabat Zinn (MBCT), Marsha Linehan (DBT), Steven Hays (ACT), or Paul Gilbert (CFT), are not the philosophical aspects of our daily living as much as, a covert focus on training the attention with the purpose of affect regulation.
What do all CBT these therapies have in common, would be a topic worthy of a whole new article, please continue to read…
Disclaimer: this site and article are not intended as a self-help manual; the intention with all NA-CBT articles is to help and to develop knowledge. All case studies described are a combination of facts and very little fiction from different sources including personal clinical experiences. Similar work and other great resources for inspiration, can be found on Ted – education, Brene Brown, Roz Shafran, Christine Padesky, Donald Meichenbaum’s research on resilience, and others.
This particular article contains might describe real life situations for learning and authenticity purposes, it may also follow anonymised cases who received NeuroAffective-CBT … this is all part of a series of free handouts offered to students on doctoral or advanced training programs in Integrative-CBT; as already explained, certain details have been changed in order to maintain anonymity.










Completely agree with this actually, thanks again D.
LikeLiked by 1 person